Sara Whittingham MD
March 17, 2025
Pisa syndrome is a condition where a person’s body starts leaning significantly to one side, usually without them realizing it. It often appears in people with Parkinson’s disease, especially after years of living with the condition. Some describe it as feeling like their muscles are pulling them sideways or like their body just won’t stay upright when they walk.


Many people notice their leaning gets worse after walking a certain distance or when they’re tired. For some, it happens mostly when standing still, while others find it worsens with vigorous exercise. One person shared that they lean so far they almost touch the ground, making activities they love—like running—much harder. Others say their shoulders and hips are uneven, and they only notice the lean when someone points it out or when they see themselves in a mirror.
Doctors aren’t entirely sure why Pisa syndrome happens. It might be due to changes in the brain’s ability to control posture, or it could be caused by tight, overactive muscles on one side of the body. In some cases, Parkinson’s medications might even play a role. The good news is that it can sometimes be improved with the right approach.
Treatment options vary. Some people find relief with Botox injections, which relax the overactive muscles that contribute to the lean. Others swear by daily stretching and targeted physical therapy, though some say traditional therapy doesn’t help much. A few have tried dry needling (similar to acupuncture) to release tight muscles. One person even joked that, as Parkinson’s warriors, they often have to figure out solutions on their own and then teach their doctors what works!
Though Pisa syndrome can feel discouraging, many who have it remain determined to keep moving forward. Staying active, finding the right therapies, and making small adjustments—like taking breaks before the lean worsens—can make a difference. While more research is needed, people living with Pisa syndrome are proving every day that it’s possible to adapt and keep pushing forward.
References: This article is a compilation of a discussion that took place on The Parkinson’s Fight Club Facebook group initiated on March 17, 2025 by Michael Quaglia. Names and images have been used with permission.



I have several examples but this shows it the best. I have done this extremely starting in the middle of races and worsening as time goes on. It’s also very painful and you absolutely cannot straighten up. I tried walking aids etc and nothing helped. I have had it off and on since 2016/17, with and w/o running. I usually did not even notice it until someone mentioned it to me or I saw a shadow. Then the pain would begin. The pain in these photos was unimaginable. If I hadn’t had my friend with me as a guide I would have certainly quit. Here’s a last photo at the finish line.- Rhonda Foulds
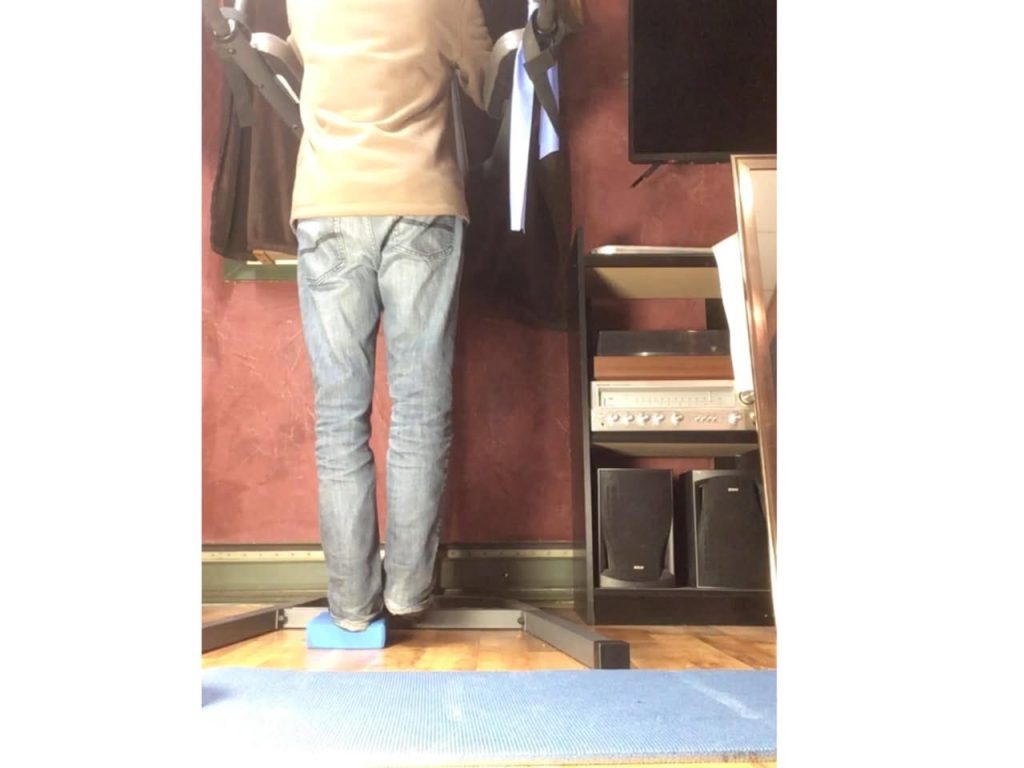
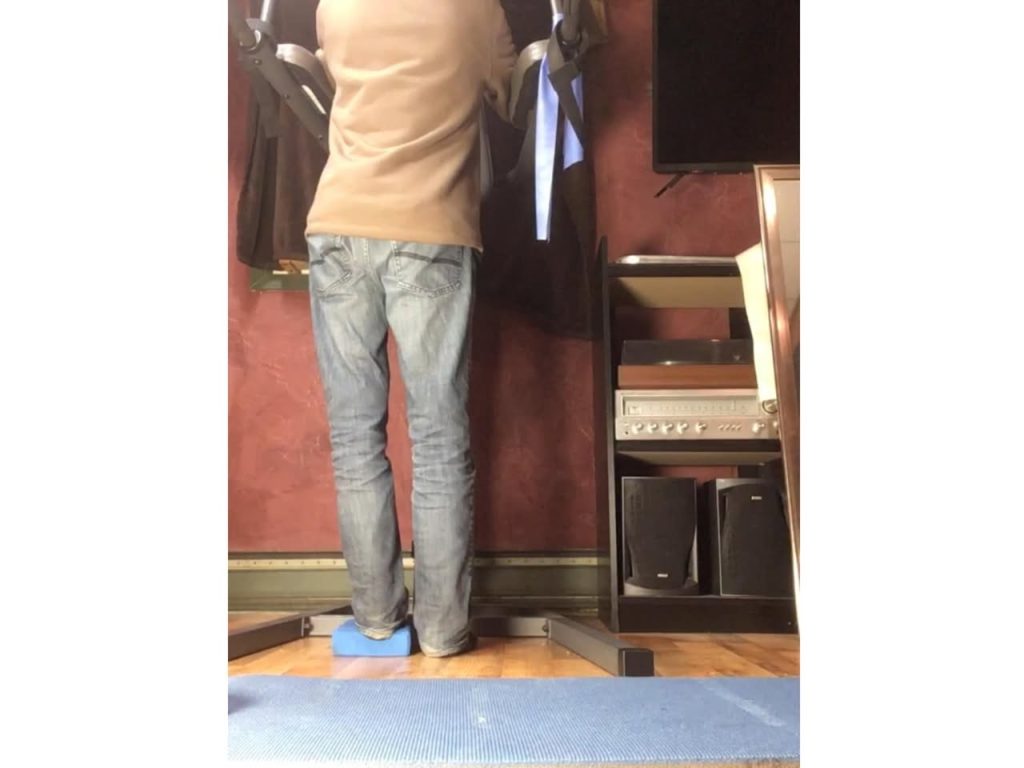
I find this simple but complicated exercise works for me.
With this exercise I use a block no higher than 2 inches, my knee on the block never bends. With my dropped leg I make sure my heal touches the floor. The only joint that moves is the hip. Note how this exercise also works my spine. As usual, check with your doctor if this is good for you. — Robert Emberly
💡 What Causes It?
Doctors aren’t entirely sure what causes Pisa syndrome, but several factors seem to contribute:
• Rigidity: Stiffness in the trunk or one side of the body can pull the posture out of alignment.
• Dystonia: This movement disorder causes involuntary, prolonged muscle contractions that can lead to abnormal posture, including sideways leaning.
• Muscle Compensation: The body may overcompensate for tightness or weakness on one side, creating imbalances.
• Medication Side Effects: Some Parkinson’s medications may contribute to postural changes.
• Neurological Changes: Damage to parts of the brain responsible for posture and spatial awareness may also play a role.
• Multiple System Atrophy (MSA): A related condition to Parkinson’s, MSA can also cause Pisa-like symptoms.
⸻
🔍 Recognizing Other Postural Changes
While Pisa syndrome specifically refers to sideways leaning, it’s not the only postural issue people with Parkinson’s may face:
• Stooped posture with rounded shoulders
• Forward head tilt (the chin juts forward)
• Uneven hips or shoulders
• Reduced range of motion in the trunk or back
Sometimes these changes happen slowly, and it’s only when others point them out—or when photos reveal the lean—that they become noticeable.
⸻
🛠 How Is Pisa Syndrome Managed?
There’s no one-size-fits-all fix, but many people find some relief through a combination of therapies. Options include:
✅ Physical Therapy
• Focused on posture, balance, and strengthening underused muscles.
• May include stretching, trunk rotation, or core exercises.
• Regular PT can help prevent worsening and build awareness.
✅ Medication Adjustments
• If symptoms are linked to side effects, changing the dose or type of Parkinson’s medication may help.
• Always consult a movement disorder specialist before making changes.
✅ Botox Injections
• Used to relax overactive muscles pulling the body to one side.
• Can be effective when dystonia is a contributing factor.
✅ Dry Needling or Acupuncture
• Some people have found relief through these methods, which may reduce muscle tension.
✅ Assistive Devices
• Walkers or trekking poles can improve posture and balance.
• Wearable posture sensors may provide real-time feedback.
✅ Daily Exercise
• Core strengthening and posture training are essential.
• Activities like Pilates, yoga, or tai chi can increase body awareness and balance.
⸻
🧭 Tips for Moving Safely with Pisa Syndrome
• Lead with your foot, not your upper body, when turning.
• Shift your weight fully before taking the next step.
• Avoid quick pivots—turn your whole body slowly and with control.
• Take breaks before the lean worsens during long walks.
⸻
💬 Real Talk from the Community
Many people share that Pisa syndrome tends to show up when they’re rushing or tired. One person said, “He doesn’t lean all the time—mostly when he’s in a hurry.” Another noted that therapy helped a little, but they had to try multiple approaches to find what worked.
A few have joked that they’re “teaching their doctors” what really helps, after trying Botox, stretching, and dry needling. And although it can be discouraging, many emphasize the importance of staying active, adjusting expectations, and keeping a sense of humor.
⸻
🧡 Final Thoughts
Pisa syndrome can feel like one more frustrating challenge in an already complex disease—but it doesn’t mean the end of independence or activity. With the right tools, support, and persistence, people with Parkinson’s are proving every day that they can adapt, advocate, and keep moving forward—lean and all.
If you or your care partner notice signs of leaning, talk to your neurologist or physical therapist. The earlier it’s addressed, the better the outcomes may be.
You don’t have to stand up straight to stand strong. Keep fighting.

Finally, someone is taking up the problem ofPisa syndrome. I’m so glad to have a reference. I’m really tired of teaching my doctors about this. This is an exact description of what’s happening to me. Mine started about 15 years after my diagnosis.